Art and medicine have been the two great recurring themes in my family. One of my great-grandfathers was Joaquim Vayreda, a famous 19th century landscape painter, whose works hang in the National Art Museum of Catalonia. My sister, who is known simply as Pilarin, is also a nationally known and much-loved artist. She has illustrated hundreds of children’s books and has won many awards.
While the art gene appears to run deep in my family, the gene for medicine appears to run even deeper. It was first on display with another of my great-grandfathers, Antoni Bayés i Fuster, a skilled physician remembered primarily for his groundbreaking studies of medicinal waters. He was the first of a line of physicians that has spanned six generations including my grandfather, my father, myself, three of my children and my grandson.
Maybe art and medicine are more closely related than some believe. Medicine is a science, but it is also an art, or at least should be approached as such. I have always felt that it is incumbent upon physicians to not only perform accurate diagnoses, but also to embrace the art of providing emotional support to our patients and their families.
Trying Years
The emotional support I enjoyed during the very trying years of my early childhood undoubtedly played a key role in shaping the person I would become. I was born in Catalonia in 1936, just 4 months before the Spanish Civil War broke out.
The years that followed were excruciatingly difficult for Spain and Catalonia. My father was largely absent during the war years, because he did not want to participate in a civil war. My determined mother fought to take care of our family, helped by my father’s parents with whom we lived.
Although the war ended in 1939, the harsh years continued through the 1940s. I was fortunate as I had wonderful friends and the school I attended, San Miguel de Vic, was unusually liberal for the time. School became an oasis; a paradise where I could play sports and study maths and science under the tutelage of some very knowledgeable professors.
Predestined
As I grew, the decision to pursue a career in medicine became easy. You might say that I was predestined – the only boy in town who lived with a father and a grandfather who were both physicians. I had always been motivated by the desire to help people, and I saw that my father and grandfather were happy, despite their heavy workloads.
At the University of Barcelona, I threw myself fully into my studies, and finished at the top of my class, but I was unsure where I would go from there. At the time, the possibilities for young physicians in Spain were limited. My father had trained in Switzerland and specialised in pulmonology, but he recommended that I pursue cardiology. It turned out to be great advice. Thanks to recent advances in cardiac surgery, catheterisation and electrophysiology, cardiology was a speciality with a future – my future.
This was the late 1950s and I spent the next 2 years studying at the School of Cardiology and working as an intern at the Clinical University Hospital of Barcelona. The school had recently been founded by four young cardiologists. At the time, the physicians who knew how to auscultate patients and read an ECG were cardiologists. It was there that I met two of my most important mentors, Miguel Torner Soler and Ignacio Balaguer.
Prof Torner Soler was a remarkable, mostly self-taught, expert in congenital heart diseases with an exceptional gift for clinical observation and keen semiotic skills. He later became the president of the Spanish Society of Cardiology.
Prof Balaguer, who also later served as the president of the Spanish Society of Cardiology, would become a pioneer in epidemiology. He sensed that ischaemic heart disease would be a future plague and in order to treat and prevent coronary atherosclerosis, its risk factors would need to be identified. This was at a time when most people assumed that heart disease was practically untreatable and unpreventable, and non-smokers were considered old-fashioned reactionaries. Essentially, the only drugs available to treat heart diseases were digitalis, nitroglycerin and mercurial diuretics.
Along with its magnificent professors, this humble school had been making significant contributions to cardiology research both nationally and internationally. Between 1955 and 1958, researchers at the school published four original articles in the American Heart Journal, then the most prestigious cardiology journal in the world.
Wanderlust
This was the exciting and nurturing atmosphere I found myself in after embarking on my new career in cardiology. But in my early 20s, I had an urge to see the world. That was not easy to do in Franco’s Spain and very few had the opportunity to leave. Of the 100 students in my class at medical school, only three of us had this privilege. Fortunately, I had relatives who lived in Gerrards Cross, Buckinghamshire, near London, and for the first time in my life, I ventured far from home.
In London, I studied at the Royal Postgraduate Medical School at the Hammersmith Hospital and attended clinical demonstrations at the National Heart Hospital. The demonstrations were given by Paul Wood, widely considered the greatest British cardiologist of his time. Postgraduate physicians from all over the world were travelling to London to learn from him. I was very impressed by what I saw and heard in London, but I was also pleasantly surprised to discover that the remarkable School of Cardiology in Barcelona was not far behind.
New Responsibilities
My time in London was short but memorable. After only 8 months, I was offered a position in Barcelona I felt I could not turn down. I returned to take on a cardiology fellowship at the University Hospital and, shortly thereafter, a consultancy at the Hospital for Cardiac Diseases.
My life had changed in another important way, too. It was in England that I met the love of my life, Maria Clara. She and I were from the same town and she was also studying abroad. We met only once in England, but we decided we would see each other again when we came back to Spain.
When I returned, I knew it was time to take on adult responsibilities. Maria Clara and I were married when I was 25 and she was 20. We have been married for 56 years and she has been a great and constant source of strength and stability for me.
In the years that followed, I became intrigued by the potential of Holter monitoring, a technology that had been developed in the US. I was fascinated by the prospect of being able to record many hours of heart activity and being able to interpret the results in just a few minutes. Having been attracted to non-invasive cardiology in general, I loved the technology and I could sense that it was a great step forward. I became one of the first cardiologists in Europe to use it.
Another Turning Point
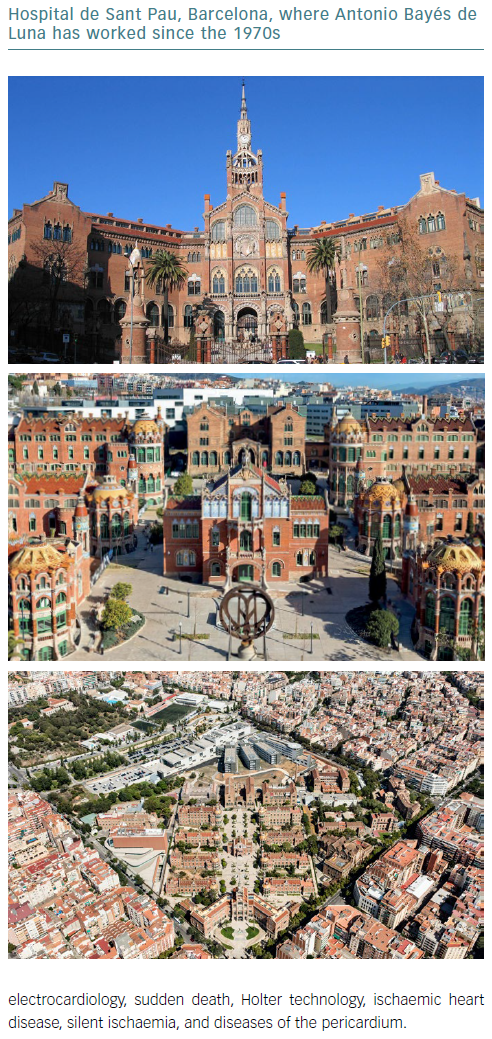
By this time, the School of Cardiology had moved to a larger space in the port of Barcelona, which provided improved technological resources. But the new location did not meet our growing needs and we were unable to treat the rapidly growing incidence of ischaemic heart disease. In 1970, we moved to the fantastic Hospital de Sant Pau.
Along with its beautiful architecture, the Hospital de Sant Pau has a rich history steeped in the finest medical tradition, and it brings out the best in those who are fortunate enough to practise there. I have been blessed to spend more than half of my life at Sant Pau, where I became Chief of Cardiology. It has afforded me great freedom of movement as I have pursued my research – especially in electrophysiology, electrocardiology, sudden death, Holter technology, ischaemic heart disease, silent ischaemia, and diseases of the pericardium.
Among other things, I have had the time and resources to write the textbook Clinical Electrocardiography, which was published in Spanish in the 1970s and in English in 1993, and has now been translated into nine languages. It is widely regarded as one of the definitive books on the subject. When I was training and learning about electrocardiography, I found the subject so challenging that I decided to write a book for myself as I wanted to be sure that I understood the subject.
Electrocardiography has been a passion of mine. In 1973, I became the chief of the Electrocardiography Laboratory at St Pau Hospital. A few years later, I organised the First International Symposium on Diagnosis and Treatment of Cardiac Arrhythmias and the first symposium on Holter monitoring, both held in Barcelona.
My interest helped lead to a breakthrough study that was published in the American Heart Journal in 1989. Philippe Coumel, Jean François Leclercq and I studied tapes of patients who had died while wearing Holter devices. We found that the most frequent causes of sudden death were ventricular tachyarrhythmias (84% of cases) and bradyarrhythmias (16%). Only a small percentage of patients presented ischaemic ST changes. And among the patients who died due to bradyarrhythmias, the cause was more likely to be sinus depression than atrioventricular block.
Bayés Syndrome
My interest in surface electrocardiography led to another study in the 1980s, published in the European Heart Journal, and for which I am probably best known. We demonstrated that patients with advanced interatrial block (AIB) were more likely to develop AF, and that the longer the P wave duration, the stronger the association.
Adrian Baranchuk, who is from Buenos Aires, but practises and teaches in Canada, coined the name Bayés syndrome to describe this association. The syndrome is now well-known, and AIBs are recognised not only as risk markers of AF and stroke in patients with heart disease and we are trying to demonstrate its association with cognitive impairment and dementia.
I have continued to devote most of my research to AIBs and their clinical implications, especially if it is necessary to provide anticoagulation for these patients to prevent stroke and cognitive impairment.
Championing ECG
One of the paradoxical effects of the enormous expansion of medical knowledge over the years has been a decrease in training and research in the field of surface ECG and ECG interpretation. During specialty training, medical students are now expected to learn at least the basics of many other diagnostic techniques, including cardiac interventions and imaging modalities, and they may get the impression that those are more current and important than a diagnostic technique that is more than a century old.
As time goes on, there are fewer mentors who can provide basic electrophysiological instruction. Most ECG concepts were developed more than 50 years ago and now there is a lack of knowledge, even among cardiologists, about newer aspects of ECG diagnostics and how they correlate with invasive and non-invasive imaging.
A few years ago, Miguel Fiol-Sala and I founded what we call the “passionate ECG club” with the support of the International Society for Holter and Noninvasive Electrocardiology. Our aim has been to convey its importance and foster the same passion and enthusiasm in young cardiologists. Prof Fiol-Sala and I also co-authored the book Electrocardiography in Ischemic Heart Disease: Clinical and Imaging Correlations and Prognostic Implications.
Recently, several colleagues and I helped demonstrate the current relevance of ECG when correlated with contrast-enhanced cardiac MRI. We discovered what we referred to as the end of an electrocardiographic dogma: for decades, a prominent R wave in V1 had been considered the sign of a posterior MI. But in fact, the appearance of a prominent R wave in V1 reflects a lateral MI in most cases.
I am also proud to have been part of a study that showed colchicine is the most effective drug to prevent recurrences in patients with pericarditis.
Hearts and Minds
I have been fortunate to lead a rich and rewarding life. In one hand, I’ve had a happy family life with my first passion – my beloved wife and 5 sons (1 boy and 4 girls), who are already in their 50s and have given to us 13 maravelous grandchildren. We are fortunate to live all in Catalonia between Vic and Barcelona, and are able to meet frequently in our family house in Vic. Furthermore, my second passion is my professional activity as a cardiologist.
I had the opportunity to be the founder and first president of the Catalan Society of Cardiology in the 1970s, and I was president of the Spanish Society of Cardiology in the 1980s.
As president of the World Heart Federation in the 1990s, I had the idea for the first World Heart Day and published the first White Book of World Cardiology. I fervently believe that the developed world has a duty to spread its knowledge to developing countries.
Finally, I have been president of the International Society of Cardiovascular Pharmacotherapy, a society that exclusively focuses on all aspects of treatment of heart disease with drugs.
These days, I am slowing down a little. I still go to the hospital every day with the same joy, but I do not take on the worries I had in the past. I can leave the administrative duties to the younger folks. Although Maria Clara and I might otherwise be inclined to rest a bit more, our grandchildren have an energising effect.
For our 50th anniversary, we went to the Olympic Games in London. I have always loved sports, especially the Olympics, and have always been fascinated by those who figure out new and better ways to do things.
At the 1968 Olympics, a gangly civil engineering major named Dick Fosbury came out of nowhere to win the gold medal in the high jump by using a technique no one had ever thought of before. He threw himself over the bar backwards and head first. Now, the Fosbury Flop is the standard for all top high jumpers.
I am also a fan of the great Spanish tennis player Rafael Nadal because I so admire the intense effort he puts forth on the court. Roger Federer may be a better player technically, but Nadal’s great heart pushes him to perform at the same level, which is a wonderful example for young people.
Our minds and our hearts are what set us apart as a species. For me, the greatest joys have come from using my mind to better understand how all of our hearts function, along with the opportunity to share the knowledge I have gained not only with my colleagues in Catalonia and Spain, but also through my books and articles, to many other countries.