Atrial fibrillation (AF) is the most common arrhythmia and is associated with increased risk of stroke, heart failure and mortality.1 Following increased therapeutic options for AF, an update in guidelines for management of AF has been published. A symposium, chaired by Karl- Heinz Kuck, Hamburg, Germany, was held at the European Society of Cardiology (ESC) congress in Paris on the 2nd September 2014. It aimed to inform cardiologists of the 2012 ESC guidelines and also to foster a “shared care” approach between electrophysiologist and cardiologists.
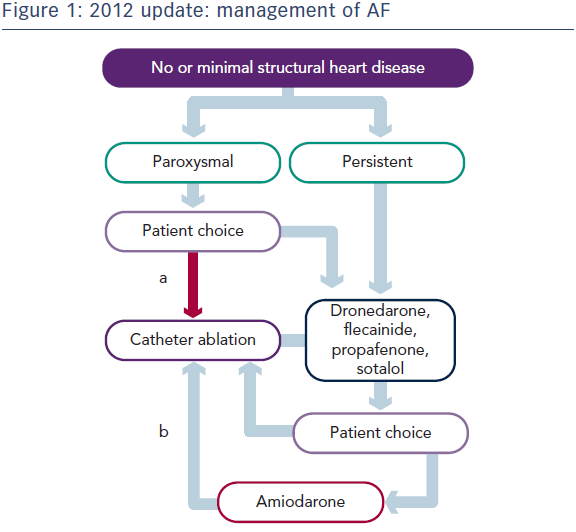
An update of the 2010 ESC guidelines for the management of AF, developed with the European Heart Rhythm Association, was published in 2012.2 The definitions of AF are: paroxysmal AF (PAF) is AF of duration 48 hours or less but a maximum of 7 days. Permanent AF is AF that persists for at least 7 days or requires a cardioversion, or long standing persistent AF lasting more than a year, as well as permanent AF in which physician and patient accept that AF should not be converted.3 The ESC guidelines have incorporated patient choice into the treatment paradigm (see Figure 1). In addition, for the first time, the guidelines state that catheter ablation is recommended in patients who have symptomatic recurrences of AF on antiarrythmic drug therapy and who prefer further rhythm control therapy (class I recommendation). Catheter ablation should be considered as first-line therapy in selected patients with symptomatic PAF as an alternative to antiarrhythmic drug therapy (class IIa). These recommendations follow a clinical trial that demonstrated that, among patients with PAF without previous antiarrhythmic drug treatment, radiofrequency ablation resulted in a lower rate of recurrent atrial tachyarrhythmias at 2 years compared with antiarrhythmic drugs.4
Application of the ESC Guidelines to Real Life Cases
In order to illustrate the challenges of AF management, Professor Schilling presented four real-world cases for discussion by a panel of expert cardiologists.
Case 1
Case 1 was a 55 year-old man with symptomatic PAF. The patient had no previous history of cardiovascular disease (CVD) or other relevant medical history. Professor Schilling proposed a thyroid function test (TFT) but not an echocardiogram; the latter would not, in his opinion, have a significant impact on patient management. The patient had a CHA2DS2-VASc score of 0 and therefore did not need anticoagulation. However, the panel considered that an echocardiogram was essential to assess the size of the left atrium, left ventricular function and whether mitral stenosis is present. If the patient had mitral stenosis, the CHA2DS2-VASc score would be irrelevant because anticoagulation would be required. Despite consensus of the panel and the audience that an echocardiogram is mandatory in this patient, this is not reflected in the guidelines.
In terms of treatment, the panel agreed that patient choice was important. Options include rate control. Depending on the frequency of AF, a conservative pill-in-pocket strategy may be preferred. The guidelines state that regular antiarrhythmics should be the first choice. Most would consider catheter ablation but would involve the patient in the decision-making process.
Case 2
Case 2 was a 35 year-old man diagnosed with AF during a routine medical examination. He was asymptomatic with no history of CVD. Professor Schilling proposed a TFT and 24-hour Holter tape to determine whether the AF was persistent rather than paroxysmal, followed by an echocardiogram to assess possible structural defects. No stroke prevention was required: the CHADSVasc score was 0.
In terms of treatment, rate control is a reasonable option. Rhythm control would not be offered because cardioversion and drugs offer no prognostic benefit. The Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) trial showed that management of AF with rhythm control offers no survival advantage over rate control and that the latter has potential advantages, such as a lower risk of adverse effects.5 Remaining in sinus rhythm was associated with reduced mortality but the use of rhythm control drugs was associated with increased mortality.6 However, if this patient had a normal heart and PAF, catheter ablation may be a better option. A registry study showed that restoration of sinus rhythm by catheter ablation was associated with lower rates of stroke and death compared with medical treatment.7 Furthermore, ablation was more successful in PAF than in persistent AF. Further clinical trial data are needed to support this.
The panel considered that clinical trial data were not applicable to this patient: he is not representative of study populations. Most agreed that a discussion explaining but not encouraging catheter ablation, would be appropriate. A significant proportion of the audience would perform cardioversion, despite the fact that there is no evidence for its benefits and evidence of harm. The panel considered that recurrence rate following cardioversion is high; it should be used in emergencies only.
Case 3
Case 3 was a 76 year-old man who presented with a transient ischaemic attack (TIA), was in sinus rhythm and had no history of CVD. Professor Schilling proposed an ECG, carotid Doppler test and echocardiogram. He would not recommend a 24-hour Holter tape; instead he would advise keeping a pulse diary. Depending on the findings of the latter, he would consider prolonged monitoring or an event recorder. A 24-hour tape has poor sensitivity and specificity for AF screening.8 Monitoring by the patient or a family member may be equally as effective at detecting an irregularity. A study of patients aged ≥55 years following a cryptogenic stroke or TIA, found that AF lasting ≥30 seconds was detected in 16.1 % of patients fitted with a 30-day event-triggered recorder, compared with 3.2 % in the control group, who were fitted with a 24-hour monitor.9
The Asymptomatic AF and Stroke Evaluation in Pacemaker Patients and the AF Reduction Atrial Pacing Trial (ASSERT) study showed that, in patients with hypertension but no history of AF, episodes of atrial tachycardia >6 minutes were seen in approximately one-third of patients and were associated with a 2.5-fold increase in the risk for ischemic stroke.10 However, these patients were all fitted with a pacemaker and there is no evidence that that successful catheter ablation reduces risk of stroke.
In terms of treatment, if AF or AF triggers were found, an anticoagulant may be recommended.
Case 4
Case 4 was a 68 year-old man with shortness of breath coinciding with new onset palpitations, a week prior to admission to the emergency room. A diagnosis of persistent AF was made. An echocardiogram would be useful to assess LV function, mitral regurgitation and left atrial size. If the patient had been experiencing AF for several years, a conservative management strategy would be advised. The echocardiogram should be performed only when the rate is controlled: a fast heart rate would impede assessment of LV function. Echocardiography can also indicate AF duration: a small left atrium is associated with short duration of AF.11 The guidelines recommend rate control and, if still symptomatic, either cardioversion and amiodarone for at least a year or catheter ablation.12 Professor Schilling prefers the latter option. He then introduced a complication: the patient had a myocardial infarction (MI) 2 weeks previously, with subsequent implantation of a coated stent. This raises issues about the use of anticoagulation. The ESC guidelines in terms of anticoagulant therapy are based on risk profiles for AF patients. However, this case presents a dilemma in how to balance the risk of stroke and stent thrombosis. An electrophysiology specialist would assess risks from the viewpoint of AF and reduce dual antiplatelet therapy, but in doing so would increase the risk of stent thrombosis. The guidelines do not address these issues. This case illustrates the importance of clinician judgement.
Discussion and Concluding Remarks
Dr Kuck began his discussion by stating that the progression from PAF to persistent AF should be a new endpoint in AF treatment and, to illustrate this point, returned to case 2. If this patient is allowed to remain in AF for 5 years and subsequently becomes symptomatic, he will be more difficult to treat as he may have structural changes including remodelling of the left atrium. This led to the question: when should catheter ablation be performed? In Dr Kuck’s opinion, as early as possible, ideally at the time of PAF to prolong the time to progression to chronic forms of AF. The ongoing Early treatment of Atrial fibrillation for Stroke prevention (EAST) Trial will determine whether rhythm control therapy, when applied early after initial diagnosis of AF, can prevent cardiovascular complications associated with AF.13
In order to demonstrate the importance of early treatment, Dr Kuck presented a study that investigated the long-term procedural success of catheter ablation in patients with symptomatic PAF and normal left ventricular function. After a median 1 procedure, stable sinus rhythm was achieved in 80 % of patients.14 By contrast, in a study of the 5-year efficacy of catheter ablation for long-standing persistent AF, success rates for single and multiple ablation procedure were 20 % and 45 %, respectively.15 Patients with a total AF duration <2 years had a significantly higher ablation success rate than patients with AF duration ≥2 years (76.5 % vs. 42.2 %, respectively). These data show that prolonging the decision to undergo catheter ablation may not be best for the patient.
In RecordAF, a worldwide prospective study, patients with recent onset AF were allocated to rate or rhythm control.16 AF progression (paroxysmal to persistent) at 12 months occurred in 15 % of patients. Patients treated with rhythm control were less likely to show progression than those treated only with rate control (11 % vs 26 %; p<0.001). Independent predictors of AF progression included history of heart failure, history of hypertension and rate control rather than rhythm control.16 In the absence of large randomized controlled trials, these data may help inform clinical decision-making. The ongoing ATrial FibrillaTion ProgrESsion Trial (ATTEST) aims to determine whether early radiofrequency ablation treatment in subjects with PAF delays AF progression compared with drug therapy (rate or rhythm control).17
This seminar has stimulated discussion between electrophysiologists and cardiologists and highlighted the need for large clinical trials to inform early treatment decisions. It may be concluded that among selected patients with PAF and no structural heart disease, catheter ablation is reasonable as first-line therapy.