Hypertension increases the risk of heart attack, stroke, kidney disease, and heart failure1 and is the leading preventable risk factor for global cardiovascular (CV) disease burden worldwide.2 At ages 40–69 years, each increase of 20 mmHg in systolic blood pressure (BP) is associated with more than a doubling of the baseline mortality rate from cardiovascular disease (CVD).3 However, despite the fact that the impact of BP on CV risk is supported by one of the greatest bodies of clinical trial data in medicine, few clinical studies have been devoted to the issue of BP measurement and its validity. Studies also lack consistency in the reporting of BP measurements and some do not even provide details on how BP monitoring was performed.4 This article aims to discuss the advantages and disadvantages of home BP monitoring (HBPM) and examines new technology aimed at improving its accuracy.
The Use of Home Blood Pressure Monitoring
Office BP measurement is associated with several disadvantages. Large variability in office BP readings have been reported, both in clinical trials5 and in the primary care setting.6 A study in which repeated BP measurements were made over a 2-week period under research study conditions found variations of as much as 30 mmHg with no treatment changes.7 A recent observational study required primary care physicians (PCPs) to measure BP on 10 volunteers. Two trained research assistants repeated the measures immediately after the PCPs. The PCPs were then randomised to receive detailed training documentation on standardised BP measurement (group 1) or information about high BP (group 2). The BP measurements were repeated a few weeks later and the PCPs’ measurements compared with the average value of four measurements by the research assistants (gold standard). At baseline, the mean BP differences between PCPs and the gold standard were 23.0 mmHg for systolic and 15.3 mmHg for diastolic BP. Following PCP training, the mean difference remained high (group 1: 22.3 mmHg and 14.4 mmHg; group 2: 25.3 mmHg and 17.0 mmHg). As a result of the inaccuracy of the BP measurement, 24–32 % of volunteers were misdiagnosed as having systolic hypertension and 15–21 % as having diastolic hypertension.6
Two alternative technologies are available for measuring out-of-office BP. Ambulatory BP monitoring (ABPM) devices are worn by patients over a 24-hour period with multiple measurements and are considered the gold standard for BP measurement.8 The average of multiple measurements at home tends to be lower compared with the measurements in a surgery5 and is more reproducible than clinic measurements.5 It also has the advantage of measuring nocturnal BP and therefore allowing the detection of an attenuated dip during the night. However, ABPM monitors are expensive and, while cost-effective for the diagnosis of hypertension, are not practical for the long-term monitoring of BP.
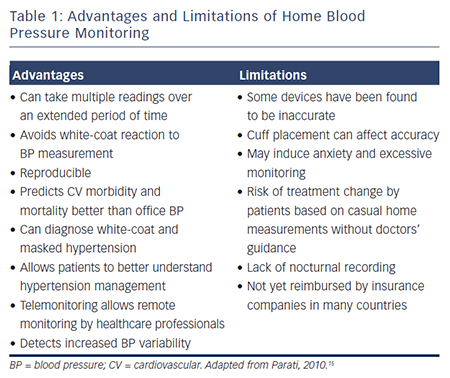
In the past decade, HBPM has emerged as an effective and convenient means of screening for hypertension,4,9 as well as being costeffective.10 Methods for non-invasive BP measurement include auscultatory, oscillometric, tonometry and pulse wave record and analysis. HBPM uses the same technology as ABPM monitors, but allows patients to monitor BP as often as they wish. The advantages and disadvantages of HBPM are summarised in Table 1. While ABPM provides BP information at many timepoints on a particular day during unrestricted routine daily activities, HBPM provides BP information obtained under fixed times and conditions over a long period; thus, HBPM gives stable readings with high reproducibility and has been shown to be as reliable as ABPM.11–13
Recommendations for the Use of Home Blood Pressure Monitoring
National Institute for Clinical Excellence (NICE) guidelines14 for HBPM recommend that when using HBPM to confirm a diagnosis of hypertension it is necessary to ensure that:
- for each BP recording, two consecutive measurements are taken,
at least 1 minute apart with the person seated; - BP is recorded twice daily, ideally in the morning and evening; and
- BP recording continues for at least 4 days, ideally for 7 days.
Measurements taken on the first day should be discarded and the average value of the remaining days after day one is discarded be used.
Except for special cases (for example, patients with arrhythmias trained in auscultatory BP measurement), the use of auscultatory devices (mercury, aneroid or other) is not recommended for HBPM.15 Monitors that use the oscillometric method are accurate, reliable, easy to use and relatively inexpensive.16 Recommendations are in place to ensure the accuracy of monitoring devices:17–19 in the UK and Ireland the Dabl Educational Trust20 and the British Hypertension Society have produced lists of validated devices.21 The European Society of Hypertension Working Group on Blood Pressure Monitoring has produced a detailed consensus document on guidelines for HBPM.15 It recommends semiautomated (manual cuff inflation) or automated electronic devices that measure BP at the upper arm as the preferred option for HBPM. Such devices are easier to use and avoid observer bias. Monitors equipped with an automated memory should prevent patients from misreporting their BP measurements. Finger and wrist devices are less accurate and are not recommended, unless brachial measurements are difficult or impossible to obtain (for example, in subjects with very large arm circumference or extreme obesity).
Advantages of Home Blood Pressure Monitoring
Reproducibility and Accuracy
It has been found that HBPM readings are often lower than readings taken in the office and closer to the average BP recorded during 24-hour ABPM.22 HBPM allows increased numbers of readings, achieves more reproducible readings than office readings and provides improved correlations with measures of target organ damage.16,23–26
A randomised controlled trial (n=555) compared manual BP measurement and automated measurement in an office setting and concluded that the quality and accuracy of automated office BP measurement was significantly higher compared with manual office BP measurement.27 A retrospective analysis of a clinical trial (n=163) compared the withinpatient variability of the different methods of BP measurement for at least 6 weeks and found coefficients of variation of 8.6 %, 5.5 %; and 4.2 % for office BPM, ABPM and HPBM, respectively. The study concluded that a week of self-monitoring was the most accurate method of measuring BP.28 Another study (n=133) found that HBP has superior reproducibility compared with both office BPM and ABPM.29
White-coat Effect and Masked Hypertension
White-coat effect, defined as elevated office and low ambulatory or home BP, can manifest with very high clinic readings. The use of automated BP measurements have significantly reduced this effect in primary care settings.27 The reverse phenomenon – i.e. normal clinic BP and elevated out-of-clinic BP – is termed masked hypertension and is associated with increased CV risk.30,31 Some studies have found that HBPM is as effective as and more convenient than ABPM in the diagnosis of this phenomenon,32,33 but others suggest that ABPM has greater sensitivity.34 A recent meta-analysis found that HPBM is particularly useful in risk stratification in masked hypertension.31 Both phenomena are relatively common, occurring in 10–15 % of patients with hypertension, but diagnosis requires physicians to be alert to the possibility, particularly with regard to masked hypertension.30,35 The European Society of Hypertension has recommended that both white-coat and masked hypertension can be diagnosed using ambulatory or home BP measurements.17
Prediction of Cardiovascular and Stroke Morbidity and Mortality
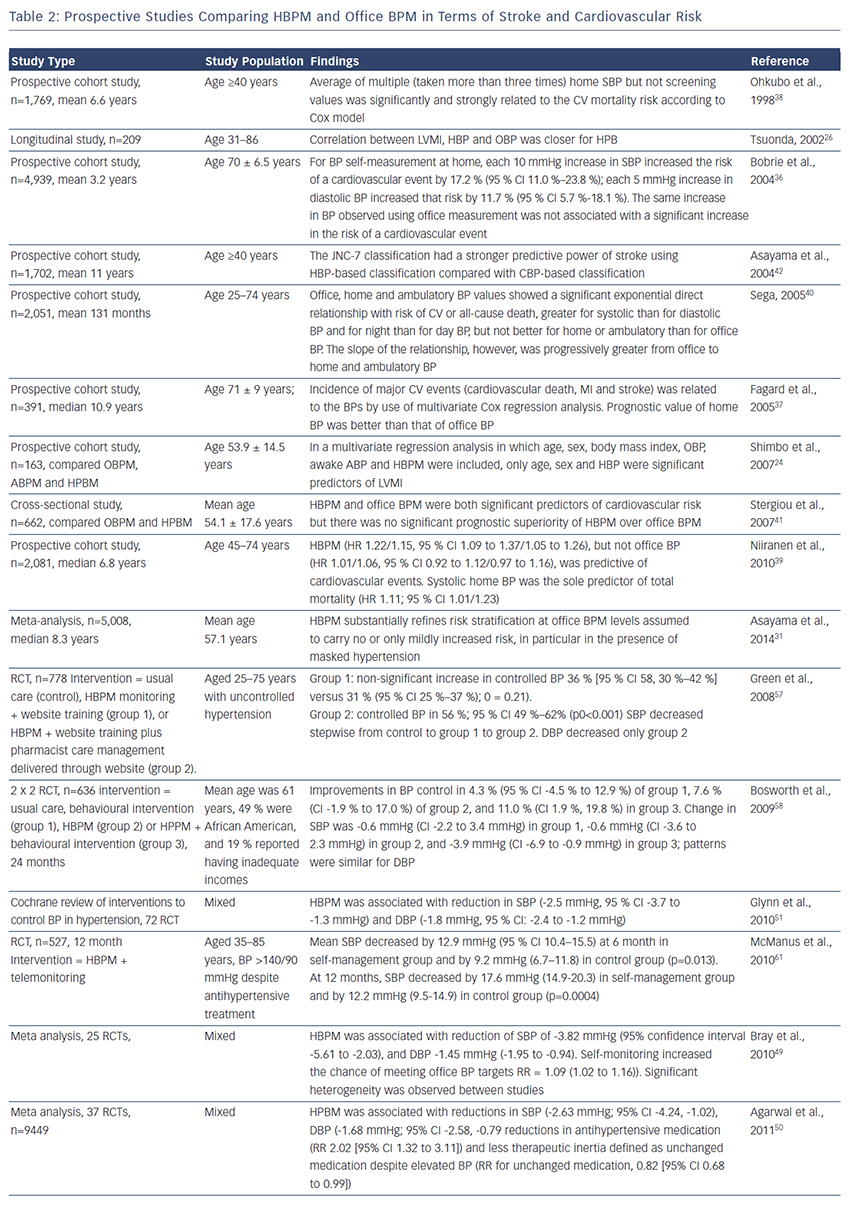
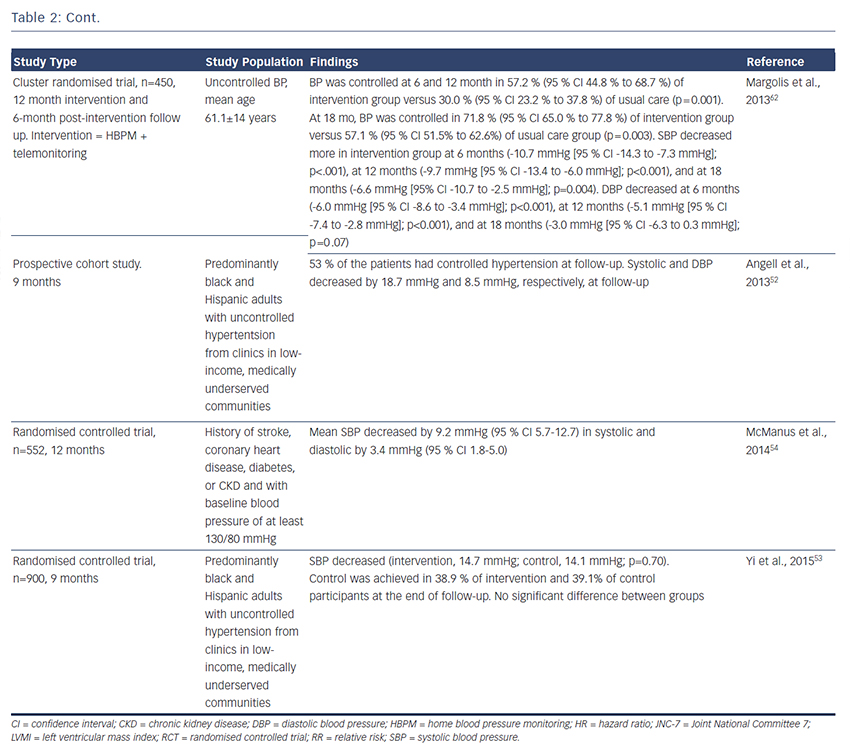
Many,24,26,36–39 but not all,40,41 prospective studies have found that HBPM predicts CV and stroke42 morbidity and mortality more accurately than office BP; the major studies are summarised in Table 2. A meta-analysis included 5,008 people who had home and conventional BP measurements and were not being treated with antihypertensive medication that would influence the prognostic outcome. Participants were stratified into five categories of BP: optimal, 120/80 mmHg; normal, 120–129/80–84 mmHg; high–normal, 130–139/85–89 mmHg; mild hypertension, 140–159/90–99 mmHg; and severe hypertension, ≥160/≥100 mmHg. At every level of BP below severe hypertension, the additional measurements obtained from HBPM improved risk stratification, supporting the use of HBPM in routine assessment of risk.31 This finding could refine risk stratification in people with optimal, normal or high-normal BP, who are not conventionally treated. A recent systematic review (19 studies) compared HBPM with ABPM in terms of outcomes including heart attack, stroke, kidney failure and/or all-cause mortality and concluded that HBPM encourages patient-centred care and improves BP control and patient outcomes.43
Large-scale studies are now investigating the optimum use of HBPM in prevention of CV outcomes. The multicentre Hypertension Objective Treatment Based on Measurement by Electrical Devices of Blood Pressure (HOMED-BP; 2001–2010) trial (n=3,518) proved the feasibility of adjusting antihypertensive drug treatment via a computer algorithm that automatically generated treatment recommendations based on HBP and suggested that a systolic HBP level of 130 mmHg should be an achievable and safe target.44 The Home Blood Pressure Measurement With Olmesartan Naive Patients to Establish Standard Target Blood Pressure (HONEST) study, a prospective observational study (n=21,591), found that morning HBP should be controlled to <145 mmHg.45
Other Advantages
Different methods of measuring BP response might clinically influence treatment decisions. A meta-analysis of more than 6,000 patients found that antihypertensive response to therapy measured by HBPM was 20 % less than office measurements.46 In addition, a clinical study found that HBPM was similar to 24-hour ABPM in assessing BP response to the antihypertensive agents atenolol and hydrochlorothiazide.47 Office BP measurements overestimated BP response compared with HBPM, with an average 4.6 mmHg greater reduction in SBP (p<0.0001) and 2.1 mmHg greater reduction in diastolic BP (p<0.0001) across all therapies.47 These findings indicate that HBPM can influence management decisions in hypertension, particularly given the relative ease of incorporating HBPM into daily activities.
Compliance and Improvement of Blood Pressure Control
Incorporation of HBPM into routine management of patients with uncontrolled hypertension may improve BP control. Several metaanalyses have shown that compared with usual care, the use of HBPM is associated with significant reductions in systolic and diastolic BP,48–51 as well as reductions in antihypertensive medication and therapeutic inertia, defined as unchanged medication despite elevated BP.50 While most studies have focused on white populations, some studies have looked at ethnically diverse adults with uncontrolled BP52,53 and highrisk patients (i.e. history of stroke, coronary heart disease, diabetes or chronic kidney disease (CKD) and with baseline BP of at least 130/80 mmHg) from clinics in low-income, medically underserved communities.54 Studies are also ongoing in stroke and at-risk groups.55
HBPM is most effective when accompanied by input from a healthcare professional, e.g. telemonitoring, whereby readings made at home are instantly relayed to a primary healthcare professional who can guide treatment along a predetermined algorithm in such a way that treatment is effected by readings obtained in a more direct manner.56–60 Numerous studies support the use of HBPM and telemonitoring,61–63 and other studies are planned.64 The use of telemonitoring avoids travel for the patient and saves time for the healthcare team. It has also been hypothesised that if patients can understand their own BP measurements and appreciate the impact of treatment, then they may be more likely to comply with medical therapy in the longer term, even if the treatment does not appear to be making them feel better.4 There is a need for clinical trial data to confirm this hypothesis.
Some studies suggest that HBPM may contribute towards medication adherence in hypertensive patients,65,66 although others have not reached this conclusion.67 NICE guidelines still recommend ABPM where possible.
Cost-effectiveness of Home Blood Pressure Monitoring
A recent cost-benefit analysis found that HBPM is more effective than conventional clinic BP monitoring in the diagnosis and management of hypertension, is easier to implement and requires less labour and capital investment than ABPM.10,68
As a result of these findings, the American Heart Association, the American Society of Hypertension and the Preventive Cardiovascular Nurses’ Association have released a statement suggesting that HBPM be incorporated into usual care.16 European guidelines also support the use of HBPM as an adjunct to conventional office management.15,69
Limitations of Home Blood Pressure Monitoring
Patient Groups
Further research is required in the clinical application of HBPM in certain patient groups; this includes children and adolescents. A systematic review of 27 studies found that HBPM has similar diagnostic value in children as in adults and appears to be a reliable alternative to ABPM monitoring in the detection of white-coat hypertension. However, systolic daytime BP readings in children was found to be lower when measured with than daytime ABPM, whereas no such difference exists in adults.70 In patients with CKD, preliminary data suggest that HBPM outperforms office BP monitoring in predicting progression to end-stage renal disease or death.71 When combined with additional support such as telemonitoring, medication titration or behavioural therapy, HBPM results in a sustained improvement in BP control. However, HBPM does not provide nocturnal recordings and therefore cannot give information on diurnal patterns in BP, which are more prevalent in the CKD population and are important CV risk factors.71 Finally, caution should be exercised in the use of HBPM in the elderly. In a comparison of Korotkoff (K-BP, the traditional means of BP measurement employed in HBPM and office methods) and Strain-Gauge-Finger-Plethysmography (SG-BP) methods, K-BP underestimated BP in 46 % of subjects with SG-BP ≥140 mmHg at age 81.72
Accuracy of Home Blood Pressure Monitors
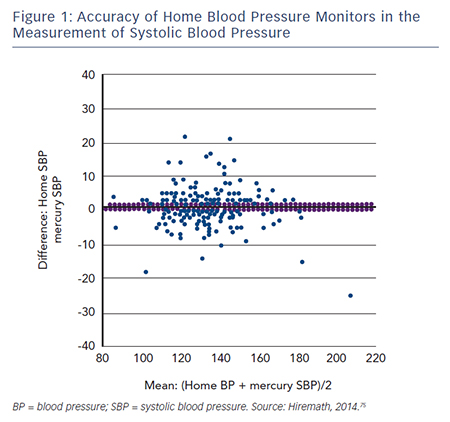
Accuracy of devices remains a limiting factor associated with HBPM. In a 2009 study to determine the accuracy of 554 automated HBPM devices, only 30 % of the devices were found to have acceptable validation, while 72 % of the automated monitors were inaccurate. The frequency of accuracy was higher among validated devices compared with non-validated devices.73 In a 2011 study, only 30 % of the 382 devices studied had been acceptably validated and 24 % of the devices were inaccurate. Upper arm devices were more accurate than wrist devices. The categorisation of upper arm devices into validated and ‘others’ showed that the validated devices were more accurate than the ‘others’.74 A recent retrospective review analysed ‘real use’ data from 210 patients attending hypertension clinics and found that 30 % of HBPM readings were >5 mmHg different and 8 % were >10 mmHg different from mercury systolic BP measurement taken in the clinic (see Figure 1). For diastolic BP, the proportions were 32 % and 9 %, respectively.75 In addition, a 2005 analysis of 30 studies found that the accuracy of most devices tends to decrease at higher BP levels.76 However, the study’s author suggested that the reported decrease in accuracy might be explained by the fact that BP is more variable at higher levels and by the use of sequential measurements.
The match between upper arm circumference and cuff size is essential to the accuracy of HBPM monitors; inappropriate cuff size has been associated with inaccuracy; studies have suggested that different cuffs should be used for BP measurement in child, adult and obese patients.77,78 The inflatable bladder of the cuff should cover 80–100 % of the individual’s arm circumference.15 The use of too small a cuff for the size of the arm can result in overestimation of BP, whereas a too large one results in an underestimation. Although standard cuffs are appropriate for most patients, in those with small (<24 cm) or large (>32 cm) arm circumference only the devices equipped with appropriate sized cuffs should be used.15 A study of six cuffs of various lengths and widths concluded a single long bladder cuff can measure BP with comparable accuracy both in subjects with large arms and in subjects with normal sized arms.79
New Technology to Improve Reading Accuracy of Home Blood Pressure Monitoring
In order to measure BP accurately, the cuff must be wrapped correctly and proper posture of the patient during the measurement is essential. Users can find it difficult to wrap the cuff in the correct position, especially if they are inexperienced. If the cuff is wrapped incorrectly then the result is less accurate. In addition, irregular pulses due to arrhythmias lead to inaccurate BP readings. Home monitoring devices equipped with automated cuff wrapping and a display indicating correct positioning have been introduced.80 These devices can detect irregular pulses that cause inaccurate BP readings. Moreover, they detect noises and wave pulses within the cuff that are caused by arm movements. These device functions may help provide more accurate BP readings.80
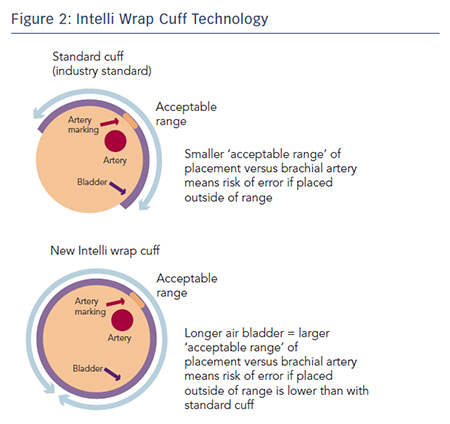
The latest development in HPBM technology is Intelli wrap cuff technology. This features a longer inflatable area within the cuff that wraps all the way round the arm. This reduces pressure loss on the brachial artery, increasing the ‘acceptable range’ of placement and thus reducing the impact of cuff placement on accuracy (see Figure 2). It is also pre-formed, enabling it to be easily fitted with one hand.
An ongoing study evaluated a validated oscillometric device (Omron M6-Comfort; HEM-7321-E) coupled with the Intelli wrap cuff in subjects (planned n=50) aged 50.7 ± 16.0 years with arm circumference 33.3 ± 4.4cm, body mass index 32.8 ± 7.9 kg/m2 and in stable clinical condition. Interim data from this study has recently been presented and shows that incorrect positioning of a conventional cuff significantly affects BP measurement results, with the greatest overestimation of BP when the bladder centre is displaced by 90° laterally or by 180° compared with the correct position. When the Intelli Wrap cuff was used, there was no significant effect resulting from cuff position. BP values obtained with the oscillometric device tended to be lower than those obtained by reference method because of relative undercuffing with the mercury device equipped with standard size cuff in subjects with a large arm circumference.81
Summary and Conclusion
The growing burden of hypertension has seen an increase in the use and availability of HBPM devices. HBPM provides extensive BP information obtained under fixed timeframes and conditions over a long period; thus, the mean values of HBP are stable and the reproducibility are high. The use of HBPM devices is cost-effective and has stronger prognostic value in terms of CV risk when compared with clinic BP measurement. HBPM is easy to incorporate into normal daily routines, can accurately assess response to hypertensive therapy and enables remote consultations by use of telemonitoring. HBPM also appears to be valuable in assessing patients at risk who would not usually be considered as potentially benefitting from treatment. However, recent data suggest that around a third of HBPM devices are inaccurate.75 The Intelli Wrap cuff technology may reduce the impact of cuff placement and arm movements on accuracy, although further studies are required to confirm this.