Aim: New antidiabetic drugs are required to be evaluated in cardiovascular outcome trials (CVOTs). Few of these are direct comparisons between new drugs, so we performed a network meta-analysis to compare the new drug classes in terms of cardiovascular outcomes.
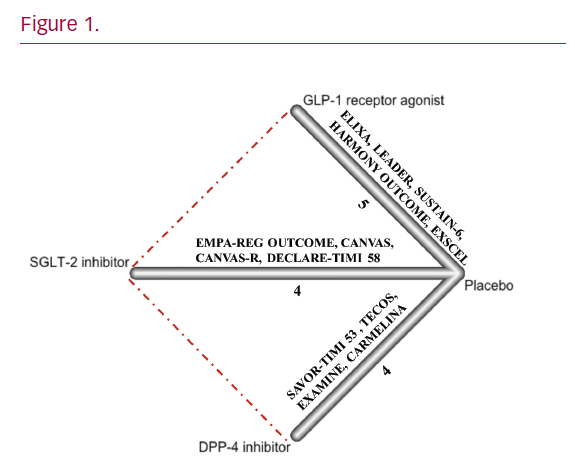
Method: We searched for CVOTs involving glucagon-like peptide-1 receptor agonists (GLP-1 RAs), sodium-glucose co-transporter 2 (SGLT-2) inhibitors and dipeptidyl peptidase-4 (DPP-4) inhibitors in patients with type 2 diabetes using major adverse cardiovascular events (MACE) and mortality as endpoints. Network meta-analysis was performed using random-effects model in R.
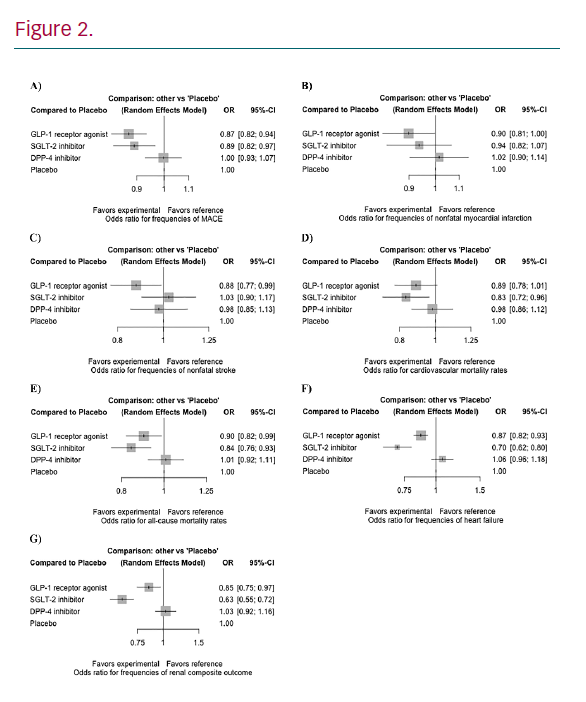
Results: 13 CVOTs with a total 116,746 patients were included (Figure 1). GLP-1 RAs and SGLT-2 inhibitors significantly lowered the risk of MACE (OR 0.87, 95% CI [0.82–0.94] and OR 0.89, 95% CI [0.82–0.97]), all-cause mortality (OR 0.90, 95% CI [0.82–0.99] and OR 0.84, 95% CI [0.76–0.93]), heart failure (OR 0.87, 95% CI [0.82–0.93] and OR 0.70, 95% CI [0.62–0.80]), and renal composite outcome (OR 0.85, 95% CI [0.75–0.97] and OR 0.63, 95% CI [0.55–0.72]) when compared to placebo (Figure 2). GLP-1 RAs reduced nonfatal stroke (OR 0.88, 95% CI [0.77–0.99]), while SGLT-2 inhibitors reduced cardiovascular mortality (OR 0.83, 95% CI [0.72–0.96]). In contrast, DPP-4 inhibitors did not significantly alter the risk of these outcomes.
Conclusion: GLP-1 RAs and SGLT-2 inhibitors both reduce MACE, heart failure, renal composite outcome, and all-cause mortality when compared to placebo. DPP-4 inhibitors did not show any cardiovascular benefits. Our findings support using SGLT-2 inhibitors and GLP-1 RAs for diabetic patients with high cardiovascular risk.